Digestive diseases account for a huge burden on the U.S. health-care industry, as they are responsible for 105 million ambulatory care visits, 14 million hospital admissions, 236,000 deaths, and $142 billion in total cost annually. These numbers are expected to grow in the coming years, primarily due to the aging population in the country, and the amount of health-care space and resources dedicated to treatment is likely to grow with them.
An increasing number of health-care systems are dedicating entire facilities to digestive health maintenance and procedures in response. Designing plumbing systems for these facilities, particularly their scope and instrument reprocessing areas, can be a daunting task even for designers familiar with them. In Part 1 of this two-part series, I will take you through the common operations and equipment in these areas and the plumbing systems involved.
Digestive health scope reprocessing areas are dedicated to the cleaning, disinfection and drying of scopes used in imaging of the digestive tract. These scopes are flexible sheaths containing imaging fibers, channels for water, air and suction, and guide wires, as shown in Figure 1.

Scopes are inserted into the digestive tract during procedures and are afterward sent to the reprocessing area, where medical staff prepares them for reuse. While workflows in these reprocessing areas may vary slightly among different organizations, they typically follow these steps:
1. Used scopes are brought in from procedure/operating areas and staged for reprocessing.
2. Medical staff begin washing the scopes by hand in large decontamination sinks with the aid of hot, cold and occasionally purified water and chemical cleaners. Scopes are brushed, flushed, leak-tested, rinsed and dried.
3. Scopes are then placed in reprocessing machines for a higher level of disinfection. The reprocessors clean, flush and disinfect them in baths of water and chemicals.
4. After high-level disinfection, scopes are moved to drying areas. Some facilities hang them on racks to dry through evaporation, but more are using drying machines fed with compressed air.
5. After drying, scopes are packaged and ready for use.
It is important to note that not all these activities necessarily occur in the same room. While facilities with smaller caseloads may consolidate all reprocessing in a single room, many are choosing to confine the first three steps into one room (dirty side) and the rest into another (clean side), with a floor-to-hard-ceiling barrier between them, as shown in Figure 2.
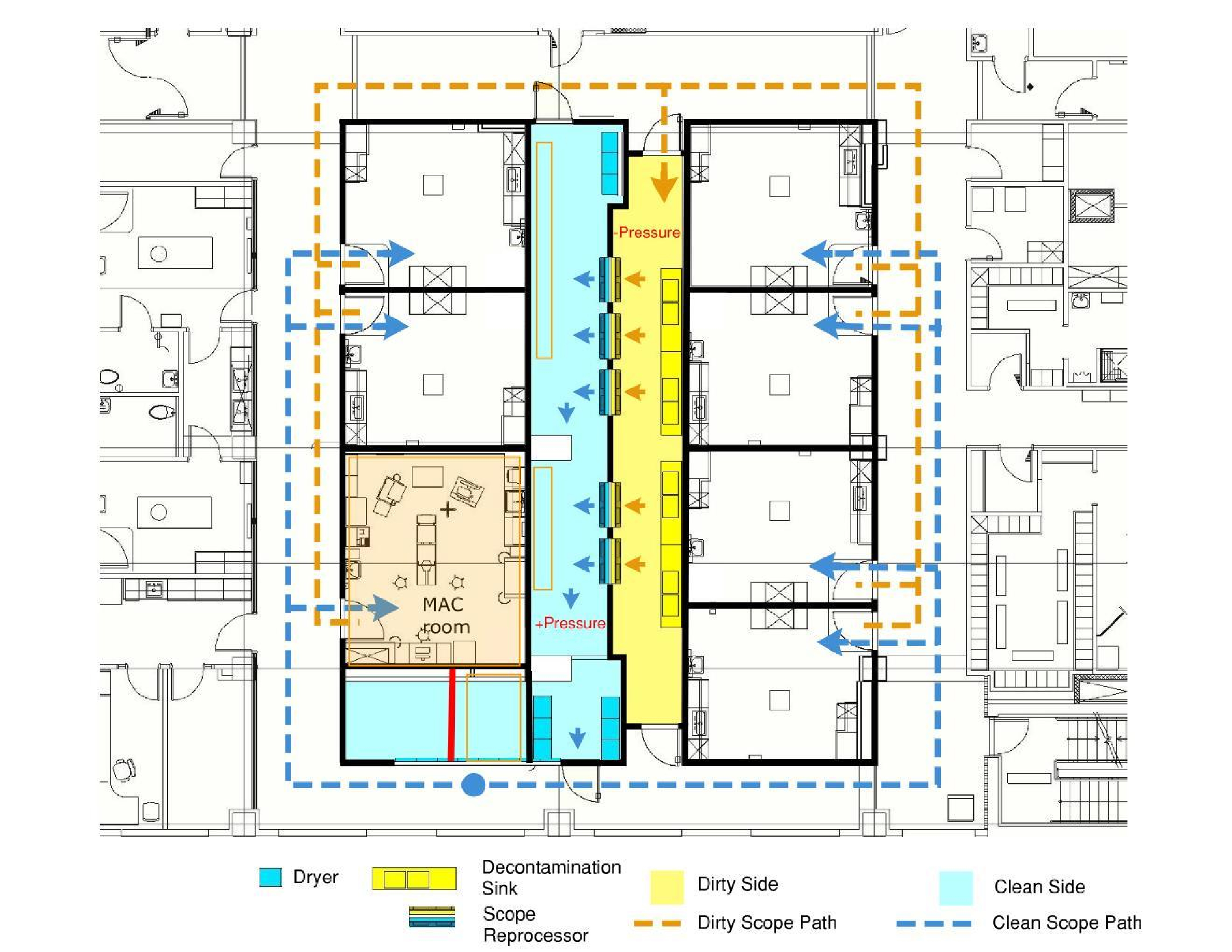
Many health-care organizations and health departments prefer a scheme similar to this since it isolates each side and reduces the risk of cross-contaminating scopes. However, if all reprocessing activities are confined to a single room, staff handling dirty scopes must not cross workflow paths with those handling clean scopes.
Common Scope Reprocessing Equipment
It is much easier to develop a design strategy for scope reprocessing areas if you have an understanding of common equipment and how it functions.
• Decontamination sinks. These sinks are the first piece of equipment used in the scope reprocessing workflow. Each sink is often staffed by a single medical professional trained in cleaning and disinfection procedures. At these sinks, staff begins cleaning the scopes of visible bodily fluids, solids and particulates.
Equipping the sinks with the correct options to do this is important, which is why health-care organizations often purchase specialized units tailored to their workflows from a medical equipment manufacturer, such as the example shown in Figure 3.

Sinks may be equipped with different combinations of the options shown in Figure 3, depending on user workflows and preferences. Most users prefer at least two sink basins (one for dirty wash water and another for a mix of clean water and detergent). A third basin may be present as well for a final rinse in purified water.
One faucet per basin is the norm, but if fewer are selected, the spouts should be allowed to swing and fill either adjacent basin. They should include elevated spouts that stay clear of users’ hands as they work. High-flow capacities capable of quickly filling the basins are crucial to keeping up with high caseloads.
Health-care organizations may equip these sinks with other options to aid the washing process. Faucet-mounted sprayers with hand valves are popular for removing solids and particulates, but some users eliminate these in favor of dedicated water guns, and still others will use both. Many decontamination sinks offer air guns for scope blowdown after washing, and most facilities use this option.
Finally, sinks with adjustable heights are becoming more common. These units allow staff to change the sink height to accommodate their stature, which increases productivity. Sinks with this feature include integral flexible drains and water supplies and do not require any other special fittings for rough-in.
• Wash accessories. In addition to the scope-washing tools and options offered on decontamination sinks, many facilities provide other devices on or near the sinks to enhance the process. Specialized detergents are crucial to cleaning. It is common to see detergent dosing units mounted on the sink or wall that release them in prescribed amounts into the basin, but they often do not require their own water supply.
Most facilities also use some type of flushing system to clean the hollow channels in scopes. Some do this by drawing water and detergent from a sink basin, pass it through the scope channels to flush out surgical fluids, and then deposit it into biohazardous waste containers that are disposed of in a central location. Systems such as these generally do not require a plumbing connection.
However, many facilities are opting to equip flushing devices with liquid waste management systems. These systems use suction to deposit biohazardous fluids directly into the building’s waste system. There are many advantages to this, such as reduced cost of biohazardous waste containers, reduced staff exposure to chemicals and pathogens, and lower risk of pathogens spreading into the air.
Liquid waste management systems are often mounted on the wall above the sink and require dedicated medical vacuum and waste connections similar to Figure 4.

• Scope reprocessors. Since scopes have sensitive internal components, they cannot be sterilized by steam and aggressive chemicals. Scope reprocessors are medical devices that, instead, provide high-level disinfection for scopes using a bath of water and specialized chemicals. Some units are small enough to sit on a countertop, but dedicated digestive health centers will generally use larger units the size of cabinets that sit on the floor, as shown in Figure 5.
If the reprocessing area is divided into a clean and dirty side, the facility will opt for a pass-through type unit where scopes enter the unit on the dirty side and are removed on the clean side. In this situation, it is imperative that floors are kept level and wall openings are kept flush to the unit so the seal between the two rooms is maintained.

After the initial manual cleaning process at the decontamination sinks, staff place scopes in the reprocessors, connect them to the reprocessor’s flushing connections and activate the cycle. The reprocessor basin fills with water and chemical disinfectant and passes the solution over and through the scopes for a prescribed amount of time. The time for the entire process varies by manufacturer but usually finishes in around 30 minutes.
After the cycle completes, the basin drains automatically to the building waste system and scopes are removed for drying.
As scopes are sensitive medical devices, scope reprocessors demand specific water temperatures, pressures and qualities. What a specific unit requires varies by manufacturer, but controls for each of these water characteristics are often needed.
For example, a common unit requires 95 F water with a 4-degree delta T, which usually means installing a mixing valve able to deliver that temperature tolerance. Most units can handle water pressures up to 80 pounds/square inch (psi) but discourage anything less than 40 psi as it interferes with cycle times and cleaning.
Finally, while most units can run on water with 10 grams/gallon (gpg) hardness or less, many manufacturers strongly encourage water softened to less than 1 gpg. Some go farther and encourage some purity level of reverse osmosis water. All supply their units with a series of prefilters on the water supply but may require another as fine as 1 micron before the water enters the machine.
Many scope reprocessors also require clean, dry compressed air. After water and disinfectants are circulated through the hollow scope channels, they are blown clean with this compressed air. This does not replace the formal drying process, though, which happens after scopes are removed from the unit.
Drains for these units can be taken indirectly to the building waste system. An open floor sink is usually the best choice, as discharge can be sudden and fast. The floor sink should be placed directly under the unit drain wherever possible, although most manufacturers offer a horizontal drain extension kit if this is not possible. Regardless, the floor sink should be kept within the unit footprint for sanitary and infection control reasons.
• Drying cabinets. After reprocessing, scopes must be completely dried to keep them free of waterborne pathogens. Some facilities do this by hanging them on drying racks. More commonly, they will instead invest in sealed drying cabinets fed with compressed air, which greatly speeds up the process and reduces the chance of contamination.
As with all other compressed air touching the scopes, it must be clean and dry. These units typically require air pressure between 60 and 150 psi and consume it at rates between 4 and 8 standard cubic feet/minute. Once the drying cycle completes, the scopes are ready for use.
As alluded to in the equipment descriptions alone, there are many things to think about when dealing with plumbing for a scope reprocessing area, along with some others that may not be immediately obvious. In the next article in this series, we will discuss the most important considerations when designing plumbing systems for these areas.
Aaron Bock, PE, CPD, GPD, LEED AP, EDAC, is a senior plumbing engineer at Erdman in Madison, Wis., and president of the Wisconsin chapter of the American Society of Plumbing Engineers. He has been designing plumbing and medical gas systems for the health-care industry since 2007, with a specific interest in waterborne bacterial control. Bock has completed more than 250 projects across the United States and is a graduate of the University of Wisconsin-Madison and Erdman’s INSPIRE leadership program.




