Time for Reflection, Part I
A review of what we have learned about dealing with COVID-19 in health-care facilities.

The COVID-19 global pandemic began this time last year, with engineers and owners scrambling to come up with ways to handle the medical gas demand we saw at the time.
There was a high demand for ventilators to treat the most severe cases of the disease. Manufacturers began to produce more ventilators at a pace we had not seen in our lifetime.
As patients were placed on ventilators, we saw a major increase in oxygen and medical air demands. As we monitored how a facility’s systems handled the increased demand, we began to see many variables in play. As we asked questions and received answers, we learned that flow rates for the ventilators were upwards of 40 liters/minute to 60 lpm due to the treatments they needed.
Kaiser Permanente and engineering firm SSR introduced a questionnaire through the American Society for Health Care Engineering to assist facilities in dealing with the increased demand on their medical gas systems. This was to help facilities get an idea of how many ventilators they could place on a system or even an area within the facility.
Makeshift emergency COVID-19 treatment facilities began popping up across the country in parking lots and parks or wherever they could obtain a large area.
Logistics for getting medical air and oxygen piped into these facilities created a demand on mini-bulk sites — portable medical air skids pulled up to feed the piping system. The piping system turned to corrugated medical gas tubing, which made for quick, cost-effective installations. Some sites used oxygen generators to address the need for oxygen instead of bulk liquid oxygen tanks.
Last summer, as ventilators rolled out across the country, we noticed that we needed to review how patients were treated. We visited jobsites to get first-hand data and found that 60 lpm was not what severe COVID-19 patients were using; it was more like 75 lpm in many cases.
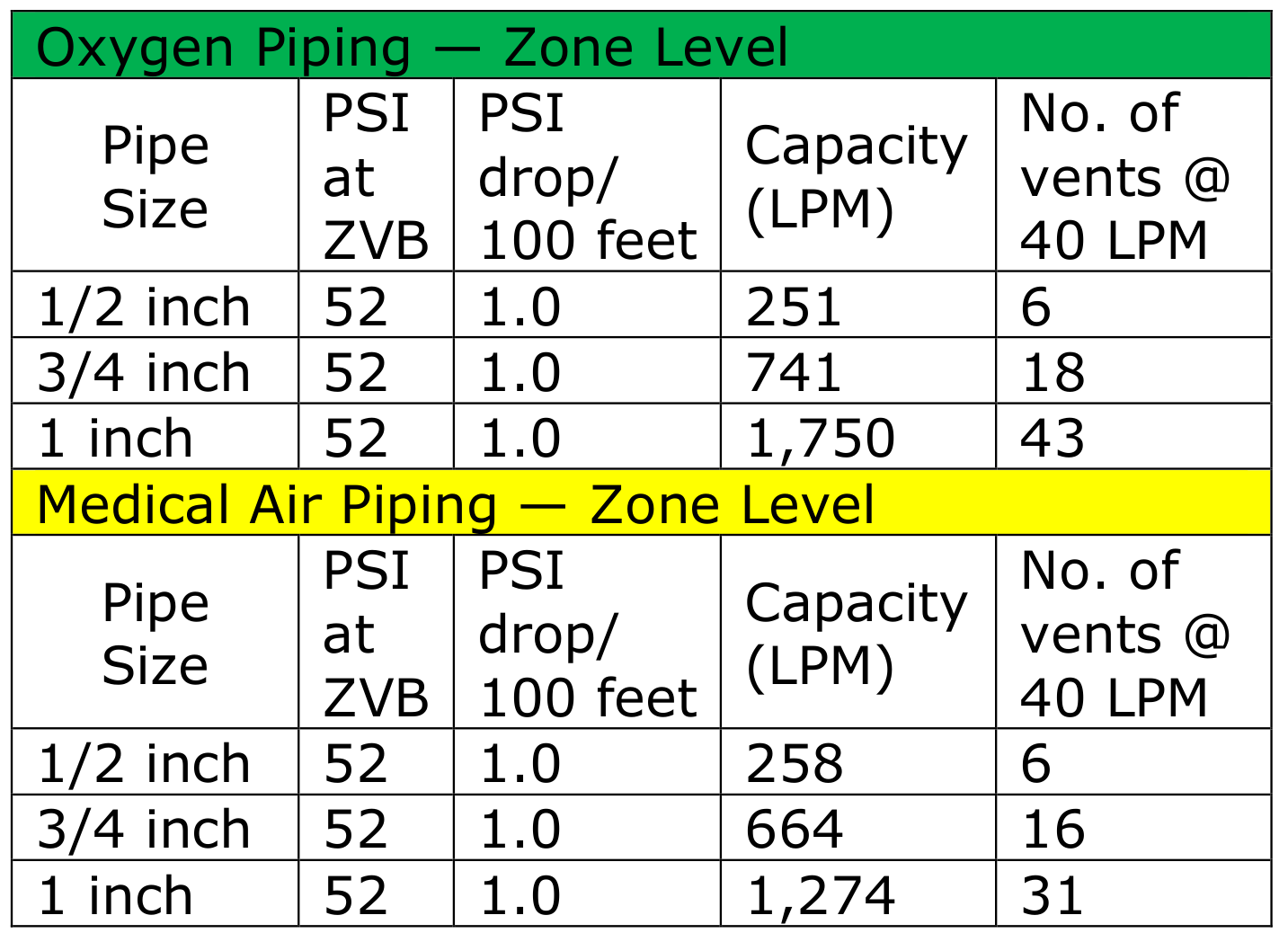
The 75 lpm came from 60 lpm ventilators with extracorporeal membrane oxygenation, delivering a possible 10 lpm and nitric at a possible 5 lpm. With this demand on 1/2-inch medical gas piping systems, it put a limit on how many ventilators could be used on this 1/2-inch line (see Table 1).
November and December, we saw a run on H cylinders and E cylinders, and even a run on liquid dewar systems. Roll forward into 2021 and we are seeing shortages on the bulk oxygen systems, with facilities not able to get more than a delivery twice a week.
High Air Flow Treatments
In December and January, we began hearing about additional treatments for patients using 75 lpm that are still being used — not with ventilators, but with Airvo air flow units. Airvos and rebreathers apparently were used from day one.
Airvos are a high flow nasal cannula using a constant flow. However, the wall connection is with coiled 1/8-inch tubing to a 70 lpm flow meter. From there, it goes out to the patient with another flow meter, but this one is 6 lpm, which they tend to remove.
Unlike a ventilator, the Airvo (see Figure 1) does not use medical air but room air. A ventilator will use oxygen and medical air to blend for the fraction of inspired oxygen the clinician is trying to reach. The Airvo draws room air from the back of the unit and blends with the oxygen.

A rebreather is very similar to a nonrebreather but with a couple of differences. Nonrebreathers have a one-way valve on incoming, including the expiration side of the mask, and typically a bag to allow for a higher concentration of oxygen
Something else to consider when determining what flow rate to use: When you speak to a respiratory therapist, she will tell you ventilators will use up to 160 lpm, but what does this mean? Do we not size or assess our oxygen and medical air systems using 75 lpm? From my experiences on the front lines, I have seen flow rates being used up to 75 lpm to 80 lpm on the high end and 35 lpm to 60 lpm on average.
That’s not to say you won’t have a ventilator use 160 lpm, but I have not seen it. Even if the respiratory therapist claims to be using 80 lpm of oxygen and 80 lpm of medical air, I have not seen it in the facilities I have been in.
The newly revised Table 2 can be used to assess a facility using the Airvo and rebreather method.
Increased Demand for Pressure, Bed Space
The increase in oxygen demands required facilities to increase their pressure at the bulk site pressure regulators to deliver 55 psi. Keep in mind that as demand increases, so will the pressure required. The inverse of this is the same as patients coming off the ventilators and Airvos — they will need to reduce the pressure back down to normal usage. It becomes a balancing act as bed counts climb and fall along with specific treatments.
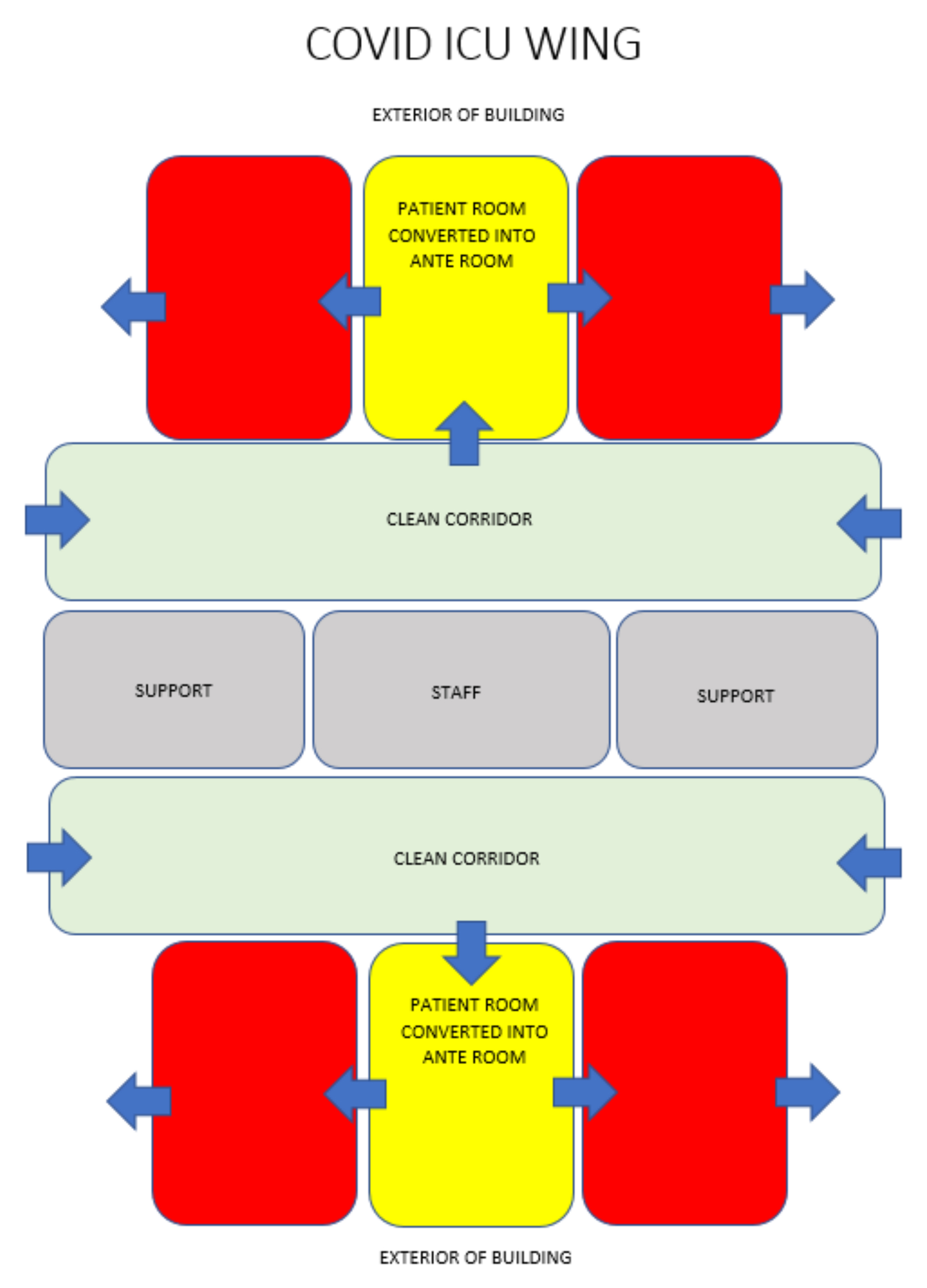
Architects also got into the mix by developing different scenarios to handle the increased demand for bed space. One of the latest concepts — converting one room into an anteroom — works well for treating multiple patients without going in and out of each patient room. This concept is geared more for larger intensive care unit patient rooms. With patient bathrooms in ICUs being considered nonessential in the future, it leaves room for doorways from room to room.
When the layout in Figure 2 shows up on your drawing board (computer screen) in the future, your medical gas requirements will likely be handled through a medical gas boom or an articulating arm. We need to make sure we request the architect or health-care planner to require larger medical gas hoses inside these booms to handle an increased flow rate. Yes, your restriction will now be down to the pigtail for the med gas outlet/inlet.
As design guides are modified and updated with pandemics in mind, the tables provided here will help in the short term
Part II will dive deeper into how we can retrofit existing facilities and design new facilities from now on. We will also walk through other possibilities, such as emergency preparedness with portables.





