How Did the Pandemic Change Our Buildings?
Not that pandemic. Think 1918.
A virus spread across the world. The medical community didn’t fully understand it, but it would come to realize that the virus could jump from person to person through the air. The first known cases were in Kansas. The year was 1918.
An estimated 500 million people caught the illness. What we now know as the Spanish Flu changed everything about normal life, including building construction. In light of COVID-19, what will be the lasting changes to building science?
In response to the Spanish Flu, History.com (https://bit.ly/2IqOIF4) explains: “Officials in some communities imposed quarantines, ordered citizens to wear masks and shut down public places, including schools, churches and theaters. People were advised to avoid shaking hands and to stay indoors, libraries put a halt on lending books and regulations were passed banning spitting.”
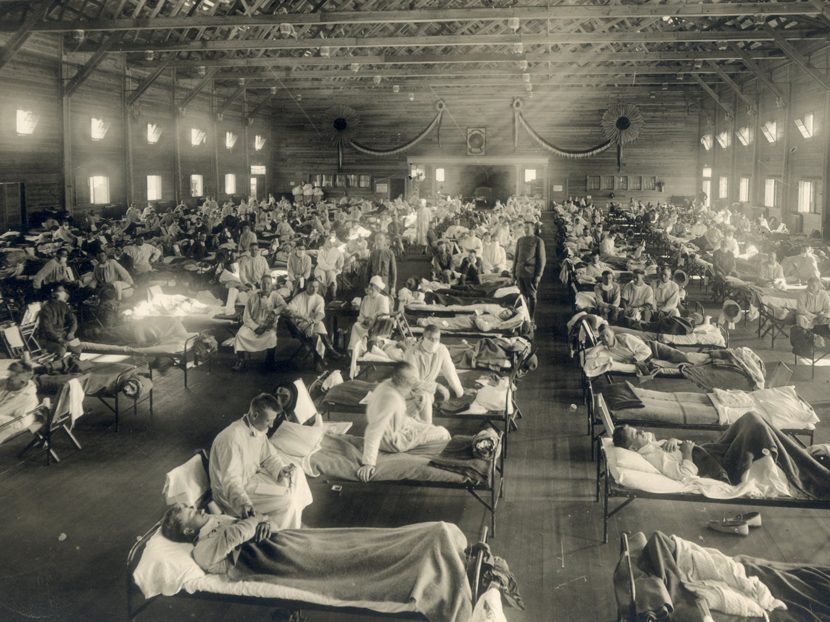
The tail end of WW I sent the Spanish Flu all over the world as troops entered new lands, which led to 40 percent of the U.S. Navy and 36 percent of the U.S. Army becoming ill from the virus. Many of the photos from the time show large, indoor spaces crowded with sick patients on cots.
In 1918, Philadelphia was one of the hardest-hit U.S. cities. A Politico article describes how public health officials in Philadelphia downplayed the virus, explained it away as the regular flu, refused to close the Navy yard where infected soldiers returned home, and even held a major parade.
“Within 10 days, over 1,000 Philadelphians lay dead, with another 200,000 estimated ill,” the article notes.
While Boston also was devastated by the Spanish Flu, it had a bit of good luck that changed how we address disease transmission today. At the Camp Brooks open-air hospital, health officials noticed the low transmission rates. (The open-air recovery treatment concept had roots in Birmingham, England, but this was a large-scale test of the concept).
A doctor named George Bodington treated patients with tuberculosis outside with smaller doses of medicine, encouraging exercise. Many doctors, then and now, would shy away from exposure to the elements without the conveniences and controls of a building. However, there was a notable improvement in patients' health outside compared to indoor spaces packed with people and little outside air.
The medical community didn’t yet understand an aerosolized virus or have tools to slow the spread. The first flu vaccines wouldn’t be available in the United States for another 22 years. The review of the pandemic in subsequent years affected how the world responded to the coronavirus that causes COVID-19. The primary area of expertise that developed from that era involved how we move air in a building.
Ventilation and humidity
Eventually, the general public in 1918 realized the air was part of the virus spread. Not knowing how a virus moves entirely, stale air was thought to be a breeding ground, if not the cause of the disease. Windows flew open. Outside air flooded in. Active ventilation wasn’t common, but the passive air exchanges to rooms with windows were (https://bit.ly/2UinNhf).
Unfortunately, another problem arose: People were now cold in their homes. Dan Holohan, industry historian, has written and spoken many times about how the Spanish Flu changed the heating systems in buildings (https://bit.ly/32DIV62). Heating system designers began load calculations assuming the windows would be open all day, which is why buildings constructed in that era may still have enormous radiators under windows.
Those buildings lucky enough to still have the large radiators can make great low-temperature hydronic heat emitters in a remodel.
Over the next century, the need for fresh air was better researched. Jumping forward to 2019, I attended a presentation by Dr. Stephanie Taylor on the relative humidity in hospitals, among other things (https://bit.ly/38MGHWb). Before COVID-19 hit, she walked the audience through her research on indoor air quality in hospitals.
Since the pandemic exploded, Taylor has become one of the busiest IAQ professionals in our industry because she possesses the data to better explain how a virus can move throughout a hospital.
Specifically, Taylor spoke about the relationship between relative humidity percentage in buildings and how it affects the transmission of airborne particles, such as viruses. One of her essential recommendations is to keep indoor RH between 40 percent and 60 percent. For rooms falling within this humidity band, particles from a sneeze or cough will settle more quickly on a surface.
While the droplets on the surface remain an issue, they aren’t blowing from room-to-room. Staying below 60 percent RH also prevents the acceleration of mold, fungus or dust mite growth.
For a deeper look at all the factors in play surrounding the transmission of infections in buildings, Taylor defined six factors:
- The number of people producing infectious droplets;
- The vulnerability of the secondary hosts (people);
- The length of the occupant’s exposure;
- The ventilation rate;
- The settling rate of infectious aerosols; and
- The survival of pathogens in aerosols during transmission.
Pandemic-specific airflow
In light of the 2020 pandemic, how do we continue to modify our buildings, especially hospitals, to have more of the open-air recovery benefits?
ASHRAE has published recommendations throughout the COVID-19 pandemic (www.ashrae.org/technical-resources/resources), and it stresses the importance of proper air movement: “Ventilation and filtration provided by heating, ventilating and air-conditioning systems can reduce the airborne concentration of SARS-CoV-2 and, thus, the risk of transmission through the air. Unconditioned spaces can cause thermal stress to people that may be directly life-threatening and that may also lower resistance to infection.”
It is a very bad idea to turn off ventilation systems entirely.
The technology and control systems are more specific in 2020, but the concept of maintaining airflow remains consistent with the 1918 vision. There are many things we can’t control about the current pandemic, but building ventilation design isn’t one of them.
If you work in the new construction design world, keep in mind that both normal ventilation standards and pandemic-specific ventilation practices might need to be control options. Can modern designs do both well?
Additionally, if you find yourself in a hospital or any building with multiple factors affecting the transmission of disease, bring your humidistat. Look for that 40 percent to 60 percent range, or pull up a chair by a huge open window. Just because we have the ventilation technology available in 2020 doesn’t mean it is being utilized properly.





